A 15 year old female with generalized anasarca
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
K.shirisha
Rollno;60,
9th semester.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
All the pictures and information had collabated from the dr.Aashitha mam and from the patient
Case discussion ;
Chief complaints;
A15 year old girl studied till 8th class and now currently working as daily wage labourer presented to the opd on 7/10/21with the complaints of
Bilateral lower limb swelling since 20days
Reduced urine output since 15 days
Abdominal distension since 5 days
Facial puffiness since 3 days
Dyspnea at rest since 3 days
Non productive cough since 3 days
Fever since 1 day
History of present illness ;
The patient was apparently asymptomatic 20days back then she developed oedema over bilateral lower limbwhich was insidious in onset gradually progressive and extended upto the thigh .it was Pitting type .no aggrevating and relieving factors
15days back she visited to hospital -1 because of oedema over legs and they said that is a kidney problem they have given medication and it was not relieved. After she developed abdomen distension ,cough, shortness of breath at restand she visited to our hospital
C/O reduced urine output, abdominal distension which is generalised, insidious in onset , gradually progressive
C/O facial puffines, swelling over hands
C/Odyspnoea at rest
C/O dry non productive cough
C/Ofever not associated with chills and rigor
She was born out of a 3rd degree consanguinous marriage. She has 2 healthy siblings. Her father expired when she was 10 years old, he was a chronic alcoholic, according to her mother who is unsure regarding the cause of his death, she attributes it to ? Respiratory Failure and Liver failure .
According to her mother, her father's elder sister had a kidney disease due to which she expired.
Past history ;
15 days back she developed a cystic lesion near her vagina which burst after she got it excised in a local hospital after which there was a serous discharge.
When she was 6 years old - she experienced cough along with dyspnea and low grade fever after which she was diagnosed to have pulmonary kochs for which she used ATT for 6 months.
Menstrual history ;
At 12 years of age - she attained menarche
Periods ; regular,cycle 28days/5days,2pads/day,noclots/pain
Personal history;
Diet ;mixed
Appetite; decreased
Bowel : regular,bladder ; decreased urine out put
Sleep; adequate
No addictions
Family history ;
According to her mother, her father's elder sister had a kidney disease due to which she expired.
General examination ;
Patient is conscious , coherent, cooperative well oriented to time ,place, person moderately built and well nourished.
Weight:55kg
Generalised edema presenet
pallor present, noicterus,cyanosis, clubbing, lymphadenopathy
Vitals;
Temperature; afebrile 98.6°
Blood pressure ;120/80mmhg
Heart rate ; 102bpm
Respiratory rate;26cpm
Systemic examination ;
CVS ;
Inspection;
Position of trachea ;midline
No visible pulsations,no raised jvp
Precordial bulge : absent
Shape of chest; bilaterally symmetrical
Apex beat ; left 5th inter costal space1cm medial to mid clavicular line
Palpation; no palpable thrills,parasternal heaves are palpable
Percussion ;
Auscultation; S1,S2 heart sounds are heared , no added murmurs,
Respiratory system;
Inspection of upper respiratory tract;
Oral cavity ; normal
Nose; no DNS,polyp
Pharynx ; normal
Lower respiratory tract;
Position of trachea; midline
Position of Apex beat; left5ics 1cm medial to mid clavicular line
Symmetry of chest : symmetrical and elliptical
Movement of chest ; normal
Palpation ;
Position of trachea,apical pulse is confirmed
No tenderness over chest wall,no crepitation s,no palpable added sounds,no palpable pleural rub
Percussion;
Resonant note heared,no obliteration on traubes space
Auscultation; Inspiratory crepts in bilateral IAA,ISA
Per abdomen;
✓Inspection;
Shape; distended due to fluid
Umbilicus; slightly retracted and inverted
Movements ; normal
No visible pulsations or engorged veins,no visible peristalsis
Skin over abdomen ;normal
✓Palpation;
Soft,non tender
No organomegaly
✓Percussion ;
Liver; dullnote heared,
shifting dullness- +
No fluid thrills,
✓Auscultation;
Bowel sounds are heared
CNS; Higher mental functions are intact
Reflexes- present
Power,muscle tone- normal
Gait- normal
No meningeal signs
Cranial nerves - intact
Sensory system - normal
On 4/10/2021
Her weight on 4/10/2021 was 55kg
Her serum creatinine was 1.3g/dl
Urine showed albuminuria 4+
Along with 4-6 rbcs and 10 - 12 pus cells, 2 - 4 epithelial cells
Her spot protein creatinine ratio was more than 7.2
Her spot urine creatinine was 150mg/dl
Spot urine protein was 940mg/dl
Her USG abdomen revealed bilateral pleural effusion
And showed raised echogenecity of Kidneys
Ascites
She was prescribed Tab Lasilactone 20/50 BD
Along with Tab Omnocortil 60mg OD
Tab Metolazone 2.5mg OD which she took for 3 days
She also has been experiencing low grade fever since yesterday night.
On examination:
Mild erythematous rash on her cheeks +
Pallor was present along with bilateral lower limb edema
On13/10/21
Investigations; on7/10/21
Hb - 10.9 gm/dl
TLC - 9100 cells/cumm
Platelets - 2.54 Lakhs /cumm
MCV - 76.6
MCHC - 35.5
Peripheral smear - Normocytic normochormic
Her blood urea here today is 206mg/dl
Serum creatinine of 2.1mg/dl
Serum albumin of 1.8mg/dl
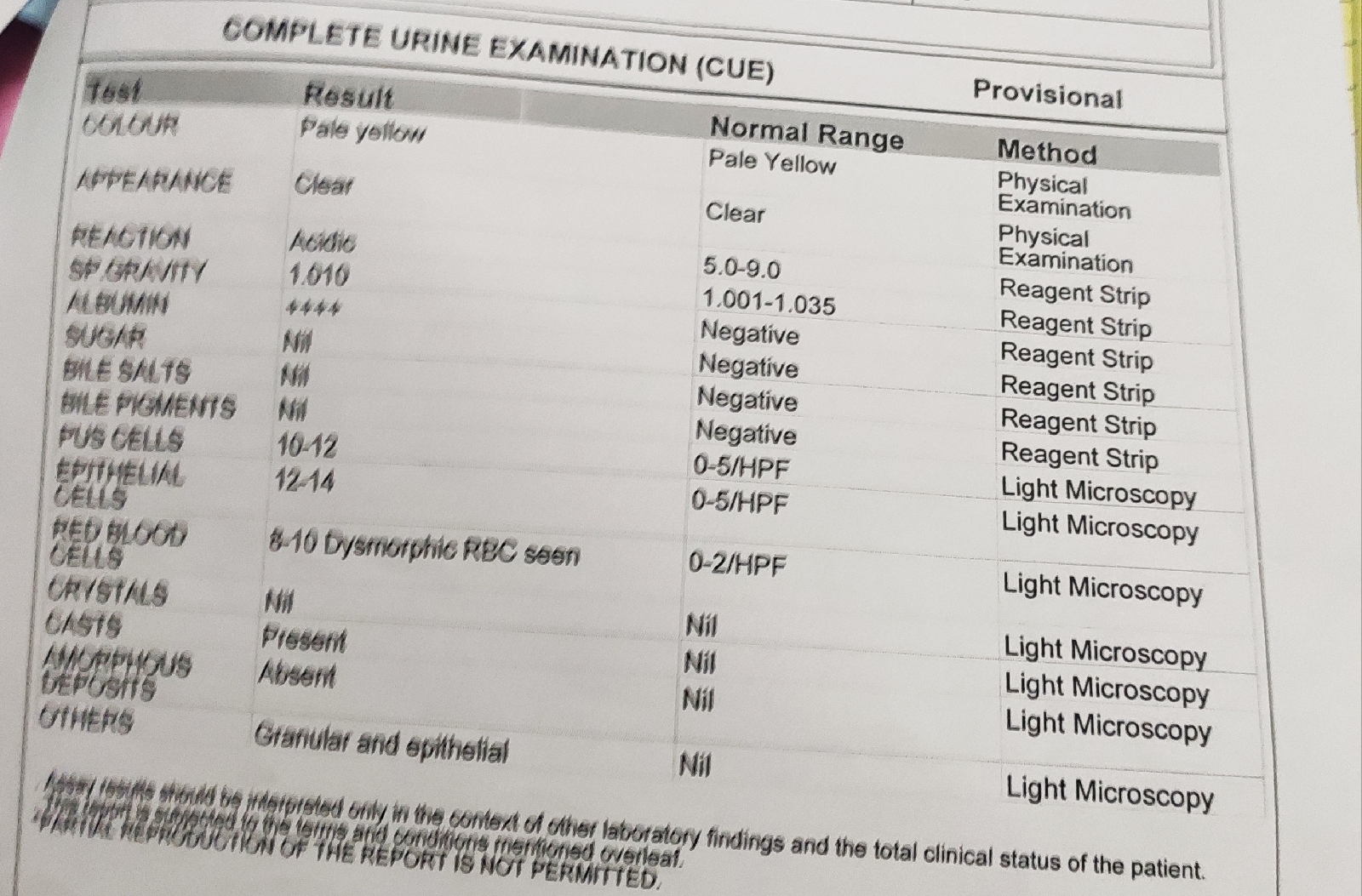
Complete Urine Microscopy:
Showing 4+ Albuminuria, 8- 10 dysmorphic rbcs, 10-12 pus cells, epithelial cells 12-14 cells/HPF
2D-echo;
Complete blood picture;
Complete urine examination;
Blood urea; elevated
Serum creatinine ; elevated
Lipid profile ; hyperlipidemia
Triglycerides;elevated
HDL cholesterol;decreased
LDL cholesterol;elevated
Ultrasound;
On obg referral : cyst was diagnosed as Bartholin gland cyst
On 8/10/21;
Pt is c/c/c
Drypcough/sob
Respiratory system ;BAE ;present,B/L basal inspiratory crepts present
P/A ; slightly distended ,non tender
On9/10/21
Pt is c/c/c
Drypcough/sob
Respiratory system ;BAE ;present,B/L basal inspiratory crepts present
P/A ; slightly distended ,non tender
On10/10/21
Pt is c/c/c
Drypcough/sob
Respiratory system ;BAE ;present,B/L basal inspiratory crepts present
P/A ; slightly distended ,non tender
On 11/10/21
Pt is c/c/c
Drypcough/sob
Respiratory system ;BAE ;present,B/L basal inspiratory crepts present
P/A ; slightly distended ,non tender
On12/10/21;
Ptis c/c/c
Respiratory system; BAE:present
B/L basal crepts present
P/A; slightly distended,no tender
Provisional Diagnosis ; Nephrotic syndrome ?UTI?CAP
Treatment;
On7/10/21;
✓Head end elevation
✓oxygen inhalation if spo2<92%
✓ inj Augmentin1.2gm/iv/bd
✓injpantop40mgiv/bd
8am-4pm
✓nebulisation-salbutamol 6thhourly
Budecort12thhrly
✓syrup ambroxyl10ml/po/Tid
✓Temp charting4thhrly
✓moniter vitals
✓strictI/Ocharting
✓tab pcm 650mg/po/Tid
✓tabcystone60mg/po/od
On 8/10/21
✓Head end elevation
✓oxygen inhalation if spo2<92%
✓ inj Augmentin1.2gm/iv/bd
✓injpantop40mgiv/bd
8am-4pm
✓nebulisation-salbutamol 6thhourly
Budecort12thhrly
✓syrup ambroxyl10ml/po/Tid
✓Temp charting4thhrly
✓moniter vitals
✓strictI/Ocharting
✓tab pcm 650mg/po/Tid
✓tabcystone60mg/po/od
On 9/10/2021;
✓Head end elevation
✓oxygen inhalation if spo2<92%
✓ inj Augmentin1.2gm/iv/bd
✓injpantop40mgiv/bd
8am-4pm
✓nebulisation-salbutamol 6thhourly
Budecort12thhrly
✓syrup ambroxyl10ml/po/Tid
✓Temp charting4thhrly
✓moniter vitals
✓strictI/Ocharting
✓tab pcm 650mg/po/Tid
✓tabcystone60mg/po/od
On10/10/21;
✓Fluid restriction upto 1.5l/day
✓salt restricted upto 2.4g/day
✓Tab.pantop 40mg/po/od
✓injLasix40mg/iv/BD
✓TABWYSLONE60mg/po/od
✓syrupAmbroxyl10ml/po/Tid
✓TABpcm650mg/po/(sos)
✓injaugmentin1.2gm/iv/Bd
✓Temp charting4thhrlyand tepid sponging if necessary
✓strict i/o charting
✓Bp/pr/spo2 charting 4th hrly
✓Grbs charting 12thhrly
✓ daily body weight monitering
On11/10/21
✓Fluid restriction upto 1.5l/day
✓salt restricted upto 2.4g/day
✓Tab.pantop 40mg/po/od
✓injLasix40mg/iv/BD
✓TABWYSLONE60mg/po/od
✓syrupAmbroxyl10ml/po/Tid
✓TABpcm650mg/po/(sos)
✓injaugmentin1.2gm/iv/Bd
✓Temp charting4thhrlyand tepid sponging if necessary
✓strict i/o charting
✓Bp/pr/spo2 charting 4th hrly
✓Grbs charting 12thhrly
✓ daily body weight monitering
On12/10/21
✓Fluid restriction upto 1.5l/day
✓salt restricted upto 2.4g/day
✓Tab.pantop 40mg/po/od
✓injLasix40mg/iv/BD
✓TABWYSLONE60mg/po/od
✓syrupAmbroxyl10ml/po/Tid
✓TABpcm650mg/po/(sos)
✓injaugmentin1.2gm/iv/Bd
✓Temp charting4thhrlyand tepid sponging if necessary
✓strict i/o charting
✓Bp/pr/spo2 charting 4th hrly
✓Grbs charting 12thhrly
✓ daily body weight monitering


















24hour urine protein??
ReplyDelete